What is trigger finger / Trigger thumb?
Trigger finger is a common disorder causing triggering/snapping or even locking of a finger or the thumb. In medical terms it also known as stenosing tenosynovitis.
The flexor tendons are like long strings that connect muscles in the forearm with the fingers and allow the fingers to bend. All flexor tendons enter a narrow tunnel as they go into the fingers.
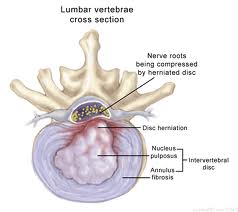
In trigger finger the entry to the tunnel is narrowed due to thickening of the outer lining of the mouth of the tunnel (also known as the A1 pulley) and a small lump in the tendon. The swelling and the lump stop the tendon from gliding freely in and out of the tendon tunnel. The tendon „catches“as it glides under the A1 pulley and the finger clicks or triggers.

In severe cases the lump in the tendon can get trapped and the finger gets stuck and locked in a bent position. Forceful straightening of the finger/thumb is usually accompanied by a painful snapping or clicking sensation.
What are the typical symptoms?
- Clicking of the finger as it bends and straightens
- This can sometimes be painful
- Locking of the finger in a bent position
- Rarely the finger can lock in a straight position
- Waking up with the finger stuck in a bent position
- A nodule can often be palpated at the base of the finger
- Ring and middle finger and thumb are most commonly affected
What are the causes of trigger finger / trigger thumb?
The precise cause is not always clear in every patient.
There are a few factors that can contribute to the development of trigger finger:
- Repetitive strain can cause swelling of tendon and pulley
- Prolonged direct pressure on tendon and pulley for example from using tools like screwdrivers can cause swelling and thickening of tendon and pulley
Some systemic diseases can have an effect on soft tissues leading to swelling and thickening like rheumatoid arthritis or gout. Patients with Insulin-dependent Diabetes are particularly at risk. Some patients seem to be prone to developing trigger finger.
What are the non-operative treatment options?
In most cases an attempt at treatment without surgery is appropriate. If an underlying cause can be identified, then treating this condition or avoiding/modifying the offending activity can make a difference. Intermittent splinting and anti-inflammatory medication sometimes help in the early stages of trigger finger / trigger thumb. Injections with steroids can be very useful and often cure the problem. Injections are usually not used more than twice in the same finger, as there is a risk of tendon rupture with excessive use of steroids.
When is surgery required and how does it work ?
Fingers that are permanently locked and/or have not responded to other treatment require surgical intervention. Surgery is best carried out as a day case under local anesthetic. A small cut is made at the base of the finger in the palm. The mouth of the tendon tunnel (the A1 pulley) is simply divided to allow free gliding of the tendon. During surgery the patient is asked to move the finger. The surgeon can then see, whether the constriction has been adequately released. Any inflammatory tissue that might contribute to the problem is removed. Fine sutures are used to close the wound; a small dressing and a bulky bandage are then applied.
When can patients start using their hand again ?
Patients can mobilize more or less straight away within limits of discomfort. The bulky outer bandages can be removed after 3 days following surgery. A small dressing is left in place to protect the wound while it heals. The wound will be checked after 10-14 days and any residual suture material will be removed. Most patients are able to use their hand for light activities within a few days. Return to work depends on the patient’s occupation and can range from a few days to 3 weeks.
What are the risks and complications involved in surgery?
Generally speaking this is a fairly simple and straightforward operation, that shouldn’t take more than 10-15 minutes. However, as with any operation there can be complications. Most of them are minor in nature and can be treated.
The scar can become tender. It may feel tight and cause pain on stretching the finger. Massaging the scar with moisturizer will help to soften the scar.
How successful is surgery?
Surgery is very successful with a low complication rate of less than 5%.
